
CNA – It often begins with a slight discomfort in your knee or hip as you get out of bed. Over time, that discomfort may develop into persistent pain, swelling, or reduced mobility – all indicative of osteoarthritis.
Like many chronic conditions, osteoarthritis is typically diagnosed only after it has progressed significantly and started to interfere with daily activities.
Researchers are striving to find ways to diagnose osteoarthritis earlier to slow or prevent some of its damage. The disease affects over 32.5 million adults in the United States and more than 500 million people worldwide.
Emerging research suggests that osteoarthritis is not solely due to wear and tear on joints, akin to tire treads wearing out.
For some, ongoing low-grade inflammation might accelerate or even cause the disease. Scientists now believe the damage begins well before symptoms manifest.
A recent study from Duke University identified blood markers in women that could indicate osteoarthritis up to eight years before X-rays detect changes in their bones.
“This tells us that there is an osteoarthritis continuum,” said Dr Virginia Byers Kraus, the study’s lead author. “You’re already on an escalator leading up to symptoms and X-ray changes way before we thought.”
WHAT HAPPENS IN OSTEOARTHRITIS?
Osteoarthritis affects cartilage, the tissue that cushions joints and allows smooth movement. This cartilage continuously breaks down and rebuilds with regular activity.
“Our body typically knows how to repair itself,” said Dr Elaine Husni from the Cleveland Clinic’s Arthritis and Musculoskeletal Centre. The joint fluid contains enzymes that remove worn cartilage, while special cells repair and rebuild it.
However, this cycle of breakdown and repair becomes dysfunctional in osteoarthritis. In some cases, enzymes may excessively remove cartilage, or the repair process might lag behind the breakdown.
Additionally, joint stress can trigger inflammation, which further accelerates cartilage breakdown. If inflammation persists, it leads to further damage.
Excess body weight is a significant risk factor for osteoarthritis, as are sports injuries, repetitive motion injuries, and inflammatory conditions like diabetes.
Over time, the cartilage loses its cushioning ability, resulting in pain, a crackling sensation, reduced mobility, and swelling. Symptoms are most common in weight-bearing joints such as the knees, hips, and lower spine, but can also affect fingers and feet.

DIAGNOSING OSTEOARTHRITIS
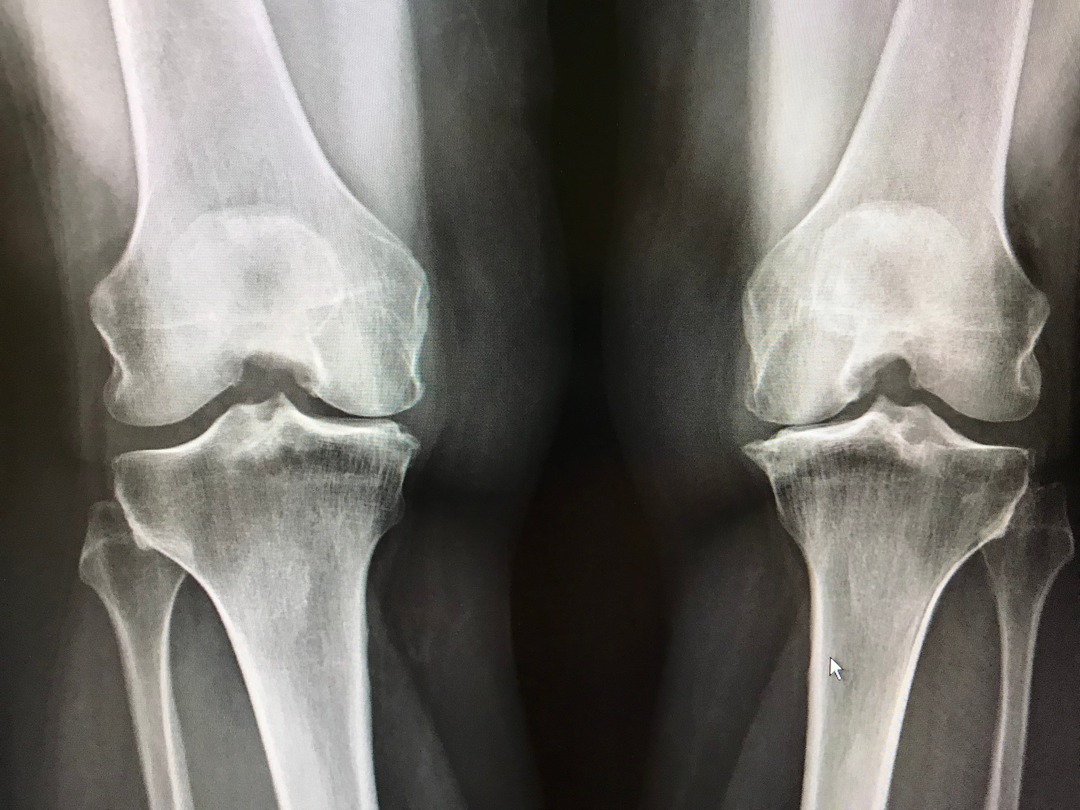
When joint pain is reported, doctors may check for swelling, test joint mobility, and perform tests to exclude other conditions. The gold standard for diagnosing osteoarthritis is an X-ray, which shows changes in joint structure. However, by the time these changes appear on X-rays, significant damage has already occurred.
Furthermore, X-ray findings do not always correlate with the severity of symptoms. “You could have two patients with the same amount of joint space narrowing, but one could have a lot of pain while the other may not,” Dr Husni explained.
Dr Kraus’s team and others are investigating biomarkers that could simplify osteoarthritis diagnosis.
While a reliable blood test might take years to develop, these biomarkers could also help evaluate the effectiveness of new treatments in clinical trials.
Currently, patients manage osteoarthritis with supportive treatments like heating pads, physical therapy, and over-the-counter medications. Dr Kraus advises that understanding osteoarthritis as a slowly progressing disease can help individuals take steps to reduce their risk or slow joint wear and tear.
Maintaining a healthy weight, staying active, and eating a balanced diet rich in anti-inflammatory foods can support joint health and overall well-being.






