THE WASHINGTON POST – The first artificial womb capable of gestating a human baby will get one step closer to reality next week – a key scientific milestone that could offer hope for the thousands of extremely premature babies born in the US each year.
The artificial placentas are fluid-filled pods intended to help struggling prematurely born infants develop much like they would in the prenatal environment.
Next week, Food and Drug Administration officials will weigh in on the safety and efficacy of the devices, as well as ethical considerations for the first-in-human studies. Part of it will be held behind closed doors, to protect trade secrets.
“This would potentially be revolutionary to neonatal care,” said George Mychaliska, a paediatric foetal surgeon and researcher at the University of Michigan.
A device by start-up Vitara Biomedical, made up of a research team from the Children’s Hospital of Philadelphia, is closest to having one ready for human trials.
Its device has already proven successful in animal studies. Premature lambs kept inside the device for up to four weeks were able to develop normally. Human trials are the critical next step in proving the artificial womb’s worth.
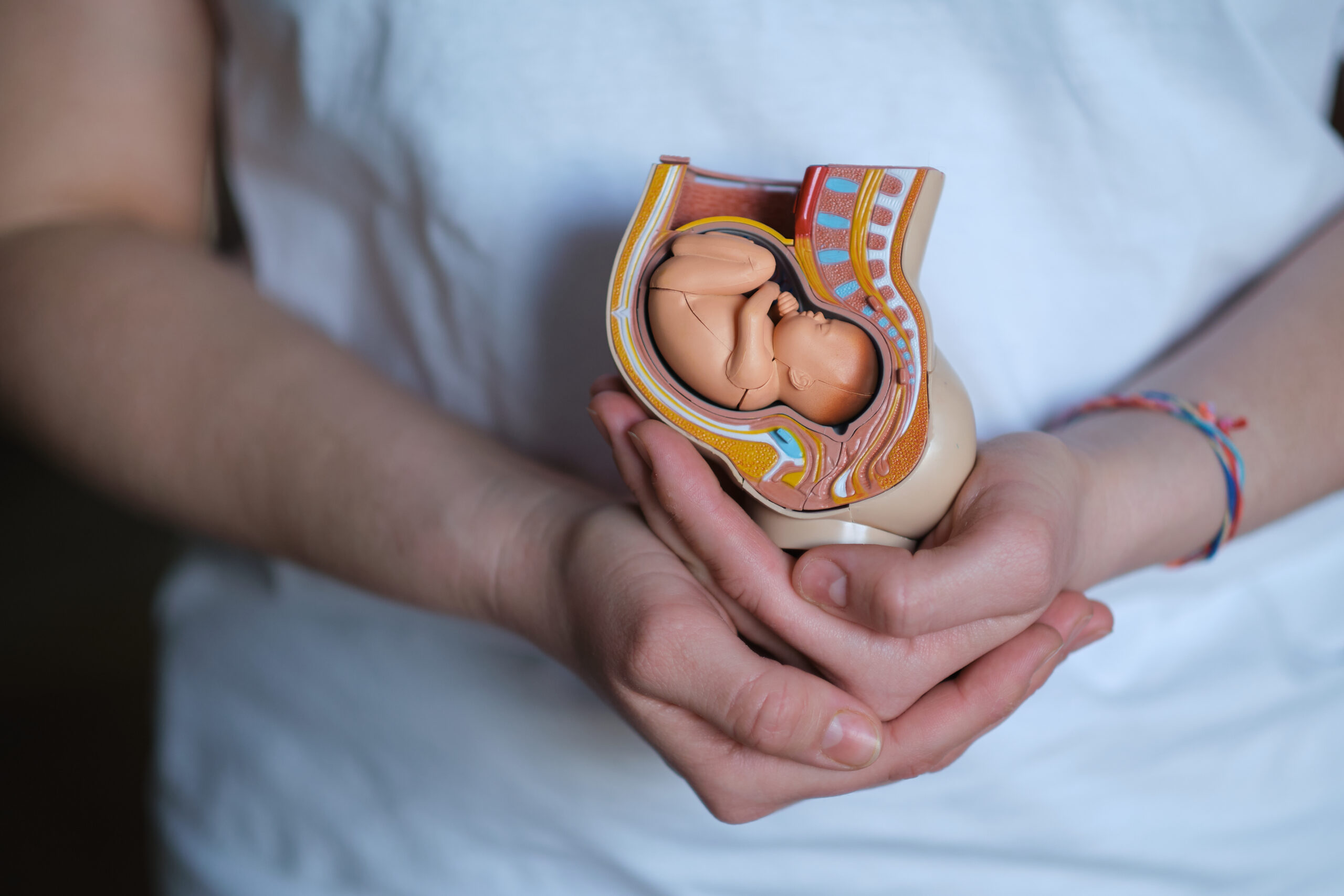
The device from Vitara Biomedical is called the EXTEND system, short for EXTra-uterine Environment for Neonatal Development. In a human womb, a foetus gets all the nutrition and oxygen it needs through the umbilical cord connected to the placenta.
The EXTEND device, intended for infants born at less than 28 weeks gestation, aims to mimic these conditions.
A physiological transition takes place when babies go through the birth canal or emerge through a C-section. The digestive system, for example, activates, and fluid drains from the lungs. Part of the challenge for scientists is to keep the infant in a foetus-like state.
The transition from a human womb to an artificial womb has to be seamless in order to stop the natural process of a foetus turning into a neonate.
So, during a C-section, tubes are inserted into the umbilical blood vessels, and the infant is immediately submerged into a biobag, a pod filled with a sterile, amniotic-type fluid.
The tubes connected to the infant’s bloodstream, called umbilical catheters, provide nutrition. A machine called an external membrane oxygenator provides oxygen.
A handful of research teams worldwide are working on artificial placenta devices, but Vitara’s group is further ahead.
The FDA has designated their technology as a breakthrough device, a status that allows novel devices to move more quickly through the regulatory process, according to a presentation last year given by Alan Flake, a co-inventor of EXTEND.
Vitara raised USD100 million of venture capital in 2022 thanks partly to billionaire-founded VC firms like First Spark Ventures, co-founded by former Google chief executive officer Eric Schmidt. (The company didn’t respond to requests for comment.)
While the technology is still some years away from being used routinely in hospitals, the FDA meeting signals that it’s closer than ever to the clinic, said Mychaliska, of the University of Michigan.
Mychaliska leads the artificial placenta research group in Michigan, the only other US team exploring this technology.
“It makes sense that if you recreate the foetal environment, babies’ survival rate will increase and, hopefully, their long-term morbidities or health consequences will be diminished,” he said.
Preterm birth is a leading cause of infant mortality in the US. A third of infant deaths in the U.S. can be attributed to being born too early, according to the latest data from the Centres for Disease Control and Prevention. Those who do survive sometimes live with life-long disabilities.
It is also a growing problem: The percentage of preterm births in the US rose four per cent in 2021, the highest level reported in at least 14 years.
That same year, preterm birth affected about one of every 10 infants. Black women are at a higher risk, with rates 50 per cent higher than white women.
In hospitals, staff of new-born intensive care units, or NICUs, often use smaller versions of approaches designed for full-term babies, like incubators and ventilators. However, complications often arise due to their fragile, underdeveloped organs.
This artificial womb is uncharted territory. Even researchers disagree on what to call the entity residing in the artificial placenta. Some call it a foetonate, others a gestateling, says Elizabeth Chloe Romanis, an associate professor in Biolaw at Durham University in the UK. Terminology is important because of the ethical and legal implications of the entity’s status, she said.
“It’s not a foetus because it’s not part of a pregnant person, but it’s also not a baby because it’s not adapted to the external environment,” she said.
The meeting will also seek to dispel misconceptions and anxieties about this new technology. When people think about artificial wombs, some envision a science-fiction future in which women’s wombs have been entirely replaced by machines. That’s not the case, Romanis said.
“It’s important to stress that this is something that’s going to help premature babies,” she said.