Singapore’s GPs are reshaping mental health care, providing accessible help, reducing stigma and fostering well-being
SINGAPORE (ANN/THE STRAITS TIMES) – At the tender age of 14, Goh Sher Jing faced a profound challenge when her mother was diagnosed with brain cancer.
As the middle child among three daughters, she assumed the role of the primary caregiver at home. Navigating through school became a haze as she attended classes, absorbing little of the lessons.
Coping with the weight of her mother’s deteriorating health, Goh resorted to self-harm, the intensity escalating with each grim update from the doctor.
Tragically, five years later, Goh’s mother succumbed to the illness, plunging Goh into a deep emotional struggle. The burden of witnessing her mother’s decline and the subsequent loss took an immense toll on her mental well-being.
“After my mum’s passing, I grappled with suicidal thoughts and attempted to take my own life, shared Goh.
Now 26, she has found employment in a retail store, but the scars of her past linger, shaping her journey through life.
For years, she kept it to herself and lived with insomnia and a poor mood. It was not until 2023 that she sought help from a general practitioner (GP) whom a friend recommended.
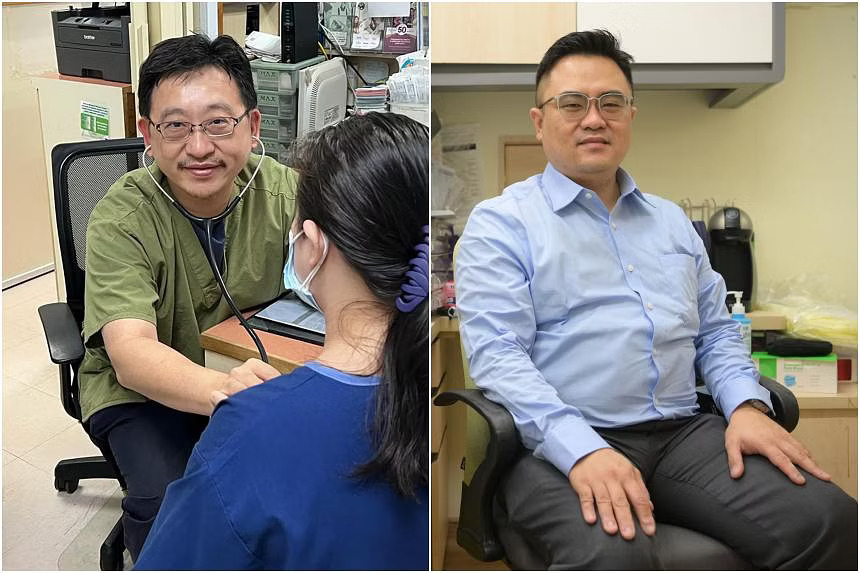
The GP, Dr Yap Siong Yew of Cashew Medical & Surgery in Bukit Panjang, spent 15 to 30 minutes with her during the first consultation, and diagnosed that she was suffering from depression, Ms Goh said.

“He gave me medication… and a book to write down how I felt every day. He wants me to release the emotions that are occupying me every day,” she said.
Until that visit, Goh thought help was available only at the Institute of Mental Health (IMH) or from expensive private psychiatrists.
But more patients like her are finding out that help may be just minutes away at their neighbourhood primary care doctor.
According to the Agency for Integrated Care (AIC), nearly 420 GPs have joined the national mental health-GP partnership programme to support patients with mental health issues since it was established in 2012. This figure is up from 122 in May 2016 and about 220 three years ago.
The network includes the 137 GPs under an older mental health-GP partnership programme at IMH, which refers stable patients to GPs in the community.
That started as a pilot in 2003, led by Dr Alvin Lum, a GP who is now the deputy director of the programme at IMH, and Professor Chong Siow Ann, a senior consultant psychiatrist at IMH. The institute has referred more than 3,700 patients to GPs in the network.
All Singaporeans are eligible for Community Health Assist Scheme (Chas) subsidies when they visit Chas GPs participating in the programme to seek treatment for major depression, anxiety disorders (including obsessive-compulsive disorder), bipolar disorder or schizophrenia.
AIC’s website has a non-comprehensive list of GPs who have agreed to the listing. Seventeen out of 24 polyclinics also offer mental health services.
In time, the pool of GPs who can treat patients with mental health issues is expected to grow. Dr Lum said he has intensified his GP recruitment efforts.
At the launch of the National Mental Health and Well-being Strategy in October, the Health Ministry said more GPs will be roped in to provide mental health services under the country’s preventive care programme, Healthier SG.

Dr Yap, who was among the first batch of GPs to complete the graduate diploma in mental health in 2010, has seen walk-in patients with mental health issues like Goh, as well as those referred by IMH and other hospitals.
He has also picked up on mental health issues among regular patients who see him for other ailments.
One of them was just seven years old. “Monday to Friday, Saturday, Sunday, stomach ache… School holidays, no stomach ache, school reopens, stomach ache,” said Dr Yap, giving a quick recap of the case. He referred the child to KK Women’s and Children’s Hospital for assessment and treatment.
“I pick up new cases and channel them to the right place for the right help. If a person is recovered or stable, I take them in and I guide them, and I motivate them,” he said.
He monitors patients even after referring them elsewhere. For example, a patient showing signs of self-harm, whom he referred to IMH, could get an appointment there only in January. So Dr Yap asked her to continue seeing him in the meantime so that he could monitor her condition.
Under the mental health-GP partnership programme, GPs can also refer patients to community help, where appropriate.

GP Jonathan Yeo of Family Medicine Clinic Chinatown said it is rewarding to help someone who is struggling with impaired function because of an underlying mental health issue, though it can be challenging and arduous to accurately diagnose and treat these conditions.
Not all patients are forthcoming with their symptoms because of the stigma attached. Some may also not recognise that their symptoms, such as headaches, insomnia, heart palpitations or abdominal pain, could be a manifestation of a mental health condition like depression or anxiety, said Dr Yeo.
“The doctor would then need extra time to tease out or decipher the underlying condition,” he added.
Still, said Dr Yap, as long as GPs have a passion for managing mental health conditions, they will be able to do it.
At IMH, the GP partnership programme has helped the majority of referred patients remain in the community, with a low relapse rate, said Dr Goh Yen Li, the programme’s director.
Dr Lum said the IMH’s GP partners have stayed with it over the past 20 years, and the institute ensures that they are able and willing to take patients.
“There’s no point bringing in a GP who is not sure (about managing a patient with a mental health condition) and might not want to see the patient,” said Dr Lum.

The patient may get scared off by the doctor, or vice versa, he said.
Goh has seen Dr Yap for a follow-up visit and is due for the next one soon. The help has given her hope of a better future.
“I know that if I suddenly think of something and can’t control (my thoughts), I have someone to get help from. I can WhatsApp the doctor,” she said.
She has a wish, which is to be able to have a good night’s sleep without the aid of medication, so that she can wake up feeling refreshed and ready for the day.